Published by: Diana Luai Awad, Dr Pharmacist on Wednesday 14. December 2022
Diuretics are one of the most important drugs in clinical practice, which have been used for over 50 years in the treatment of a number of diseases. Although they all act by altering the reabsorption of sodium in the renal tubules, diuretics differ in their mechanism of action and have different pharmacological properties and indications.
.png)
Anatomy and physiology of the urinary system
Before describing the mechanisms of action of diuretics, it is appropriate to refresh one's memory of the structure and functioning of the kidneys. The main urine-forming unit of the kidney is the nephron: each kidney consists of 1 million nephrons. These, in turn, include Bowman's capsule, convoluted tubules, and the loop of Henle.
- In the capsule plasma is filtered, as a result, coarse proteins and blood cells are retained, and the filtered primary urine enters the tubules1.
- In the proximal part of the convoluted tubules, sodium (most of it), bicarbonates, chlorine and water are reabsorbed, and protons are secreted into the lumen of the tubules.
- The descending part of the loop of Henle is permeable only to water: according to the law of osmosis, water moves in a hyperosmolar direction and is reabsorbed.
- In the thick segment of the ascending loop of Henle, sodium, potassium, chlorides, as well as magnesium and calcium are reabsorbed.
- In the distal part of the convoluted tubules, a small amount of chlorine, calcium (regulated by parathyroid hormone), sodium is also reabsorbed in exchange for the excretion of potassium into the urine (the regulator is aldosterone).
Water is reabsorbed in the collecting ducts under the action of antidiuretic hormone.
Figure 1. The basic structure of the nephron and the main points of application of diuretics
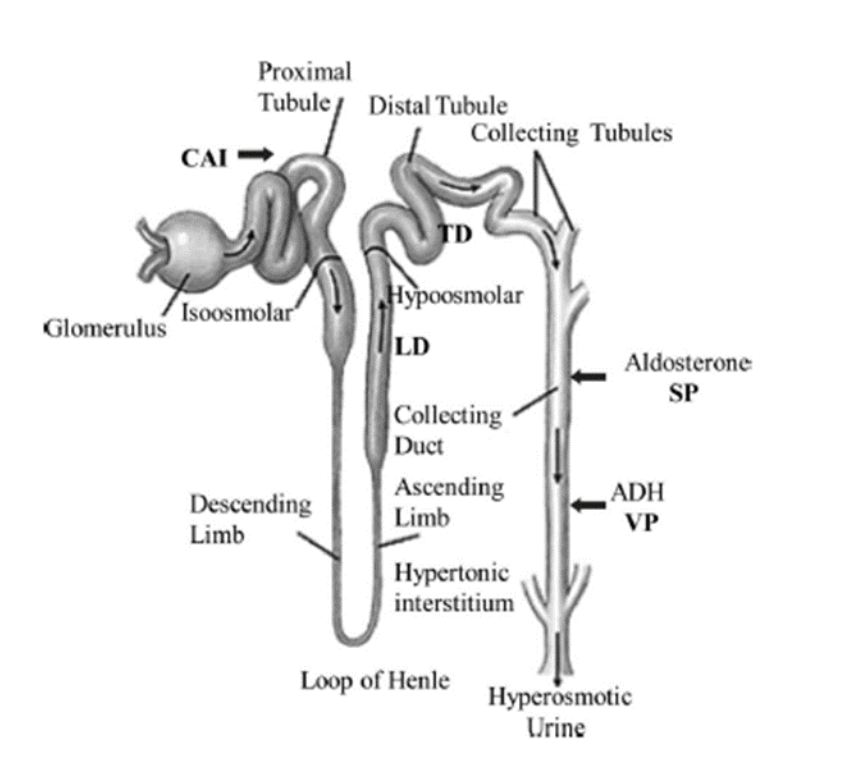
CAI, carbonic anhydrase inhibitors; LD, loop diuretics; TD, thiazide diuretics; SP, aldosterone anatagonists; VP, vaptans; ADH, antidiuretic hormone.
Table. Reabsorbent and secretory functions of various segments of the renal tubules1
|
Tubular segment |
Filtered load reabsorbed or secreted, % |
Tubular osmolality compared with plasma |
||
|
Na+ |
Urea |
Water |
||
|
Proximal tubule |
65 |
50 absorbed |
65 |
Isosmotic due to simultaneous Na+ and water reabsorption |
|
Descending thin limb of Henle loop |
0 |
50 secreted |
10 |
Isosmotic. No significant reabsorption |
|
Ascending thin and thick limbs of Henle loop |
25 |
0 |
0 |
Hypoosmotic due to active Na+ reabsorption |
|
Distal tubule |
5 |
0 |
0 |
Hypoosmotic due to active Na+ reabsorption |
|
Collecting duct system |
4-5 |
50 absorbed |
(5–24) depending on the level of ADH |
Hyper/hypo/isosmotic depending on ADH influence and medullary hypertonicity |
Classification of diuretics by mechanism of action
There are several classifications of diuretics, but one of the most famous and frequently used in practice is this classification1-3:
- Carbonic anhydrase inhibitors block the function of carbonic anhydrase within the brush border and within the epithelial cells of the proximal tubules; main purpose is the treatment of glaucoma1,2
Acetozolamide, dorzolamide, brinzolamide - Loop diuretics inhibit the Na+-K+-2Cl cotransporter (NKCC) in the thick ascending loop of Henle and are successfully used in patients with edema in chronic kidney disease and arterial hypertension1,2
Furosemide, torasemide, ethacrynic acid - Thiazide and thiazide-like diuretics inhibit an electroneutral NaCl co-transport pathway at the distal convoluted tubule and represent the cornerstone of antihypertensive therapy for many years1,2
Hydrochlorothiazide, indapamide - Potassium-sparing diuretics
- Epithelial sodium channel blocking agent inhibit the epithelial Na+ channel in the collecting duct and are mainly used in the treatment of hypertension in combination with other diuretics to correct potassium deficiency in patients without mineralocorticoid excess1,2
Triamterene, amiloride
- Aldosterone antagonists block the aldosterone mineralocorticoid receptors in the cytoplasm of principal cells of the collecting duct. Aldosterone antagonists are traditionally used for primary aldosteronism, but recent evidence indicates that they reduce morbidity and mortality in patients with heart failure1,2
Spironolactone, eplerenone
- Osmotic diuretics exerts an osmotic effect along the renal tubule, inhibiting water and solute reabsorption without interfering with tubular electrolyte transport systems and is widely used for treatment of cerebral oedema1,2
Mannitol.
Application points, mechanism of action, indications, side effects of the most commonly used diuretics1-4
|
Class1 |
Site of action |
Enzyme/channel inhibited |
Clinical uses |
Side effects |
|
Carbonic anhydrase inhibitors |
Proximal segment: acetazolamide, brinzolamide, dorzolamide, and methazolamide |
Carbonic anhydrase inhibition causes acute sodium bicarbonate diuresis |
Glaucoma, metabolic alkalosis due to loop diuretics, acute mountain sickness, hyperphosphatemia, and urinary alkalinization |
Hyperchloremic metabolic acidosis, hypophosphatemia, renal stones, and hypokalemia |
|
Loop diuretics |
Loop of Henle: furosemide, bumetanide, torasemide, and ethacrynic acid |
Active Na+–K+–2Cl2 carrier. Mutation of this carrier results in decreased Na+ reabsorption—eg, Bartter syndrome |
Acute pulmonary edema, congestive heart failure (CHF), hypercalcemia, hyperkalemia, and syndrome of inappropriate ADH (antidiuretic hormone) secretion (SIADH) |
Metabolic alkalosis, hypomagnesemia, hypocalcemia (only in hypoparathyroid patients), hypokalemia, hyperuricemia, and ototoxicity |
|
Thiazide diuretics |
Distal tubule: thiazides— hydrochlorothiazide, indapamide, chlorthalidone, and metolazone |
Active Na+–Cl2 carrier. Mutation of this carrier results in decreased Na+ absorption—eg, Gitelman syndrome |
Hypertension, idiopathic hypercalciuria, and nephrogenic diabetes insipidus |
Metabolic alkalosis, hypercalcemia, hypokalemia, hyperuricemia, hyperlipidemia, hyponatremia, hyperglycemia, and impotence |
|
Potassium-sparing diuretics |
Connecting segment and collecting tubule: aldosterone antagonists (spironolactone, eplerenone), amiloride, and triamterene |
Gradient related Na+ channel. Mutation of this channel results in increased Na+ reabsorption—eg, Liddle syndrom |
Spironolactone—primary and secondary hyperaldosteronism, CHF, and hyperandrogen states Amiloride—Bartter syndrome, Liddle syndrome, and nephrogenic diabetes insipidus |
Hyperchloremic metabolic acidosis, hyperkalemia, gynecomastia, and antiandrogen effects (with spironolactone). Nephrolithiasis, acute renal failure (with triamterene) |
|
Osmotic diuretics |
Multiple parts of nephron: eg, mannitol |
Inhibit water reabsorption in proximal tubule, descending loop of Henle, and collecting tubules |
Intracranial hypertension, prevention of renal failure after large pigment loads, dialysis disequilibrium syndrome, barbiturate intoxication |
Hyponatremia, CHF, hypernatremia with chronic use |
Bibliography
- Reddy P., Mooradian A. D. Diuretics: an update on the pharmacology and clinical uses //American journal of therapeutics.2009; 16 (1): 74-85.
- Brater D. C. Pharmacology of diuretics //The American journal of the medical sciences. 2000; 319 (1): 38-50.
- Sarafidis P. A., Georgianos P. I., Lasaridis A. N. Diuretics in clinical practice. Part I: mechanisms of action, pharmacological effects and clinical indications of diuretic compounds //Expert opinion on drug safety. 2010; 9 (2): 243-257.
- Roush G. C., Kaur R., Ernst M. E. Diuretics: a review and update //Journal of cardiovascular pharmacology and therapeutics. 2014; 19 (1): 5-13.
Colleagues, haven't you joined our PharmaCourses of MENA region Telegram chats yet?
In the chats of more than 6,000 participants, you can always discuss breaking news and difficult situations in a pharmacy or clinic with your colleagues. Places in the chats are limited, hurry up to get there.
Telegram chat for pharmacists of MENA region: https://t.me/joinchat/V1F38sTkrGnz8qHe
Telegram chat fo physicians of MENA region: https://t.me/joinchat/v_RlWGJw7LBhNGY0






